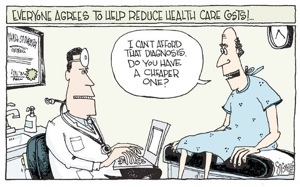
Rising Health Care Costs.
Guest post by Brandon R.
Let’s just imagine, for a second, a hypothetical patient scenario we’re faced with almost every day in the emergency department. An elderly gentleman is brought into the emergency department by his family with an exacerbation of a chronic medical condition. He’s not critically ill, but clearly isn’t thriving at home. Unfortunately he usually goes to the hospital across town, so none of his old records are accessible to you, the emergency physician. He’s also having trouble remembering how to take his medications at home, and his family is clearly nearing the end of what they can do to support him. You have no efficient method of communicating with his family doctor or home care worker. You don’t think he’s sick enough to absolutely need admission to hospital, but given the lack of ability to coordinate his care at home you have no choice but to call in a consultant to admit him to hospital.
Sound familiar? It should to anyone in emergency medicine, because scenarios like this happen every day.
In my emergency medicine residency program, we recently finished a 2 week block focusing on the administration and economics of our health care system, and it got me to thinking that this hypothetical patient scenario could illustrate many of the inefficiencies and problems our health care system is currently facing. Other countries have adopted strategies to help mitigate the problems of an aging population and rising costs, however Canada is lagging behind.
In 2004 the Paul Martin government approved a 10 year heath accord which provided a $41 billion dollar bonus to the provinces to use as they saw fit for health care, which he called “a fix for a generation.” The goal of this accord was to give the provinces the funding needed to fix their health infrastructure. The payments from this accord quietly ended last month, and at the end of the terms the provinces have very little to show for anything they did to permanently fix health care for the future. (Walkom 2014).
It’s true that the Health Accord helped in reducing wait times for hip and cataract surgery as well as radiation therapy for cancer (Health Council of Canada 2013), but now that the accord is over and the money is gone, little has been done to fix our health system for the future.
There is a looming financial nightmare facing our health care system, and we need to start making fundamental changes now or we’re going to be in big trouble. In 1984, the year the Canadian Health Act was instituted, Ontario’s government spent approximately 32% of the provincial overall budget on health care. Today in 2014, that percentage has risen to 42%. With the number of adults over the age of 65 in Ontario expected to double in the next 15 years and the rising cost of new medications and technologies, it’s projected that within the next decade we could be spending 50-80% of the total provincial budget on health care (Ontario Ministry of Finance 2010). This is clearly not sustainable.
We need to start making fundamental changes to our system, starting now, if we are going to maintain the universal health care system Canadians are proud of at even its current standard. Delaying these changes or disengaging completely from the process, which has been the policy of the federal government in recent years, only serves the risk of us falling further behind.
There are many options for what we can do to modify our existing system without compromising its basic values of universal, comprehensive, and accessible care. We need to seriously invest in an improved, integrated electronic record which properly communicates between family doctors, hospitals, and even pharmacies. Evidence from Norway’s excellent integrated electronic health network suggests that centralizing health information electronically improves efficiency, promotes better utilization of resources, improves continuity of care and communication between specialists, and improves patient safety (Snider 2012). Canada is seriously lacking in this regard, ranking 10th out of 11 developed countries, and our electronic systems are sorely lacking in compatibility between different hospitals and clinics, which frequently causes a repetition in testing and consultations (Health Council of Canada 2013).
Community-based care for seniors and long term care is still sorely inadequate, meaning patients are cared for in expensive acute-care beds in hospital instead of at home where they could be if the infrastructure was there. One in every six hospital beds is taken up by patients awaiting transfer to a long term care facility (Born 2011). There remains poor communication between primary care physicians, hospitals, and home care, leading to trouble adjusting to patient’s needs as they age and thus long term care facilities are treated as the default environment for any seniors whose needs suddenly change. There are other successful strategies of community based care that can help keep seniors at home longer and are cheaper than long term care beds, such as the On Lok Lifeways program from San Francisco since the 1970s which provides comprehensive, integrated care for seniors at home including meals, health care, rehabilitation, and social activities, yet still costs $1000 less per month than receiving similar care in a long term care home (Born 2011). We still need to invest in more long term beds, but we need to also improve our community based care to help keep seniors from needing those beds as long as possible.
Finally, we may need to look outwards to other countries to consider how they are able to contain health care costs while still providing care that is equal or superior to our own country. Recent data shows Canada’s health expenditures are 26% more per capita than the average developed nation with universal health care, although we remain a middle of the pack performer in terms of quality measures and one of the worst in terms of wait times for specialist care and diagnostic imaging (Esmail 2013). What do other countries do differently to provide efficient, more affordable, and quality care? Differences obviously vary country to country, but looking at countries which frequently are near the top of world health reports such as Japan, Italy, and France show that these countries frequently allow a certain degree of public-private hybridization to encourage competition, have small co-payments from patients to minimize overuse of the system, and employ national performance benchmarks for doctors and hospitals. Most other countries with universal health care systems also provide some sort of prescription medication coverage, which may incur extra costs but also may help reduce acute care costs for readmission for people who can’t afford their medication.
So what do we need to do to fix the situation? The first thing we need is for higher levels of government to realize the problem and start doing something about it. The provincial government is starting to take steps in the right direction by encouraging activity-based funding models and creating incentive programs for productivity, but ultimately we need the involvement of the federal government to promote nation-wide change or else we may end up with a disjointed patchwork of different health care systems with inequity between them (Boyle 2014). Paul Martin’s Health Accord wasn’t a complete failure, but what it was lacking was direction. What we need is a new Health Accord with hard targets for the provinces, such as establishing integrated electronic health records, improving community based care, and a national discussion about whether other international models of delivering health care could work in Canada. But first, we need a federal government that wants to participate in the health care discussion, and wants to talk about health care as a priority in the 2015 federal election.
Author Bio: Brandon Ritcey is a third-year resident at the university of Ottawa Emergency Medicine program and is starting an emergency point-of-care ultrasound fellowship next year. He enjoys looking at fuzzy black and white images on a screen while making wild guesses about what is going on inside of you.
Sources:
Born, Karen et al. Waiting for Long Term Care in Ontario. 2011. http://healthydebate.ca/2011/03/topic/community-long-term-care/why-have-wait-times-for-long-term-care-tripled-in-the-last-5-years. Accessed April 28th, 2014.
Boyle, Theresa. It’s a sad day for Canadian Health Care, says Roy Romanow. 2014. http://www.thestar.com/life/health_wellness/2014/03/31/its_a_sad_day_for_canadian_health_care_says_roy_romanow.html#. Accessed April 24th, 2013.
Snider, Finn. E-health helps raise quality of care in Norway. 2012. http://www.auntminnieeurope.com/index.aspx?sec=ser&sub=def&pag=dis&ItemID=606613. Accessed April 25th, 2014.
Walkhom, Thomas. Why Canada’s pricey Health Care Accord was worth it. 2014. http://www.thestar.com/news/canada/2014/04/04/why_canadas_pricey_healthcare_accord_was_worth_it_walkom.html. Accessed April 24th, 2014.
Health Council of Canada. Progress Report 2013: Health care renewal in Canada. Toronto, ON: 2013, Health Council of Canada. http://www.healthcouncilcanada.ca
Ontario Ministry of Finance. Ontario’s Long Term Report on the Economy. 2010. http://www.fin.gov.on.ca/en/economy/ltr/2010/ch3.html. Accessed April 27th, 2014.
Esmail, Nadeem. Health Care Lessons from Japan. Fraser Institute. 2013. http://www.fraserinstitute.org/uploadedFiles/fraser-ca/Content/research-news/research/publications/health-care-lessons-from-japan.pdf. Accessed April 27th, 2014.

One Comment
Leave a CommentTrackbacks